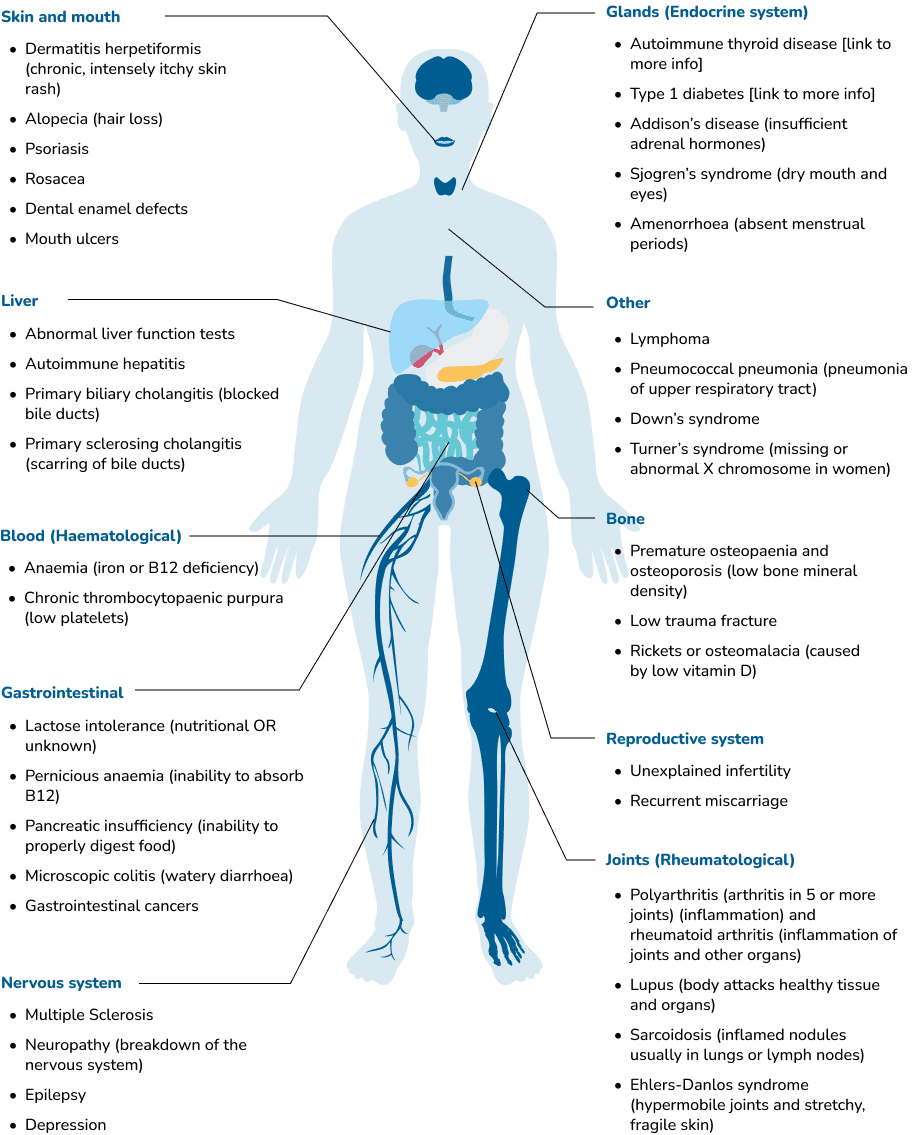
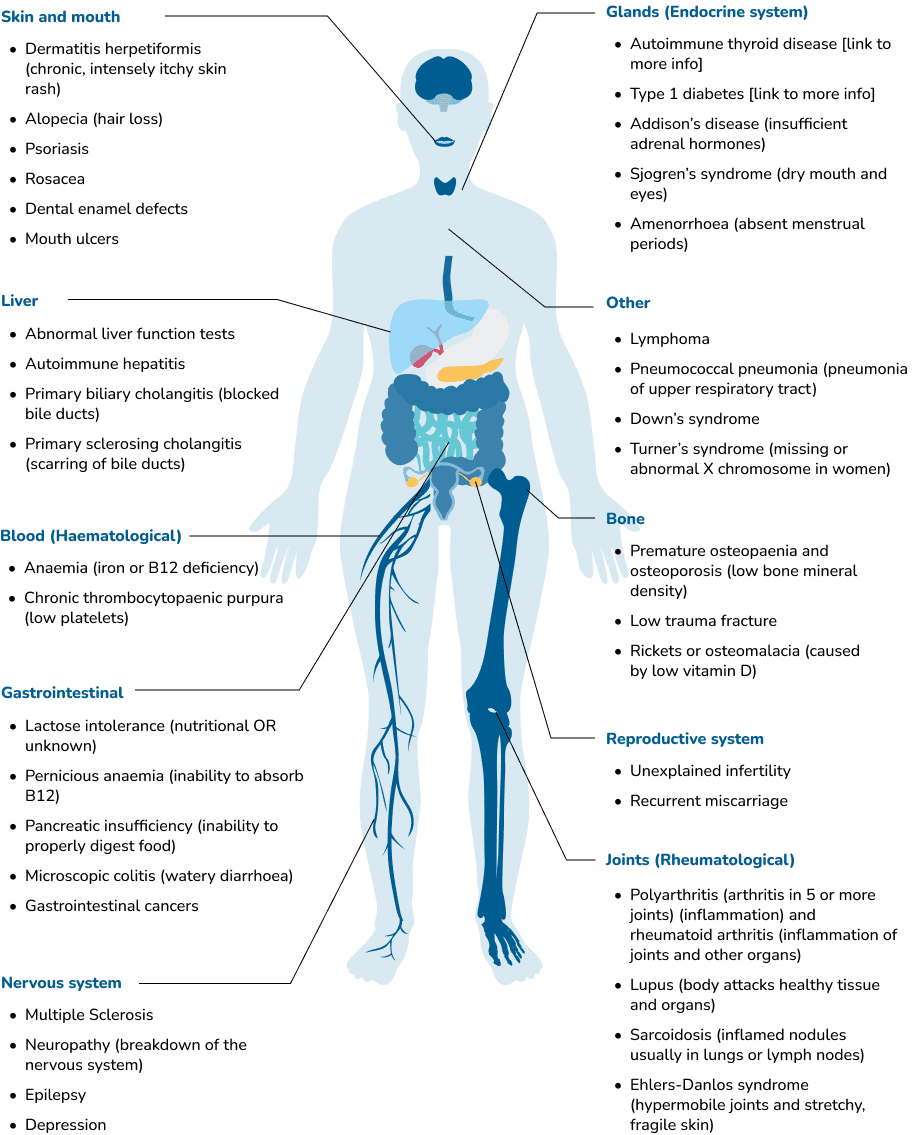
There are a range of medical conditions that can be associated (connected) with coeliac disease for different reasons:
-
Genetics – the inherited genes that make a person susceptible to coeliac disease (called HLA DQ2 and HLA DQ8) also mean they are at higher risk of other autoimmune conditions. Autoimmune diseases occur when the immune system mistakenly attacks and destroys healthy body tissue. The genetic link between autoimmune diseases mean that they often appear in ‘clusters’ i.e. multiple disorders within one person and/or a history of autoimmune disease in the family. It is important to inform your doctor if you have a history of autoimmune disease, as screening for coeliac disease should occur, even if there are no obvious symptoms of coeliac disease. There is some evidence that early diagnosis and treatment of coeliac disease reduces the risk of other autoimmune disease developing. Once diagnosed with coeliac disease, screening for certain autoimmune conditions is recommended as part of routine follow up.
-
Chronic inflammation- the inflammation caused by coeliac disease is known to cause damage to the small bowel lining. However, chronic, low-grade inflammation can also affect a variety of other organs and systems in the body such as the skin, joints, bones, liver, pancreas, thyroid gland, nervous system, and reproductive tract. It is thought that chronic, systemic inflammation plays a role in the development of many chronic diseases including cardiovascular disease, type II diabetes, cancer, depression and neurodegenerative diseases such as Alzheimer’s or Parkinson’s disease. For someone with coeliac disease, excluding gluten from the diet is necessary to reduce systemic inflammation and the risk of these long-term complications.
If your child’s coeliac antibody levels are above the normal range, this indicates they may have coeliac disease (the results of these blood tests on their own should not be used to diagnose coeliac disease without further investigation). Do not start a gluten free diet yet, even if the blood test is positive (it is possible to have a positive blood test and not actually have coeliac disease). Your child will need to see a specialist (a paediatric gastroenterologist) to confirm the diagnosis.
These tests are only reliable if your child is regularly consuming gluten. If gluten has been removed from the diet for more than around 6 weeks prior to testing, the blood test and small bowel biopsy results may be inaccurate or hard to interpret [Link to Gluten Challenge Page].
For further information on some of the more common associated conditions listed above, download one of the fact sheets below, or call our helpline on 1300 458 836.
Our Associated Conditions brochure is also available for download below or to obtain a printed copy from one of our offices, please call 1300 458 836.
Associated conditions brochure
Our Associated Conditions brochure is also available for download below or to obtain a printed copy from one of our offices, please call 1300 458 836.
Call us

Autoimmune disease
Although there are more than 80 different types of autoimmune disease, the most common autoimmune conditions associated with coeliac disease are autoimmune thyroid disease and type 1 diabetes
Know moreAutoimmune thyroid disease
Autoimmune thyroid disease occurs when the immune system attacks the body’s own thyroid gland. The thyroid gland, which is a small gland at the front of the neck, becomes inflamed and production of thyroid hormones is either abnormally increased or decreased. Often the gland becomes enlarged which is called a “goitre”.
Thyroid hormones are important for many bodily functions and metabolism. An underactive thyroid can lead to weight gain, constipation, cold intolerance and general sluggishness. An overactive thyroid can cause a racing heart, anxiety, heat intolerance, poor sleep and weight loss.
Up to 10% of people diagnosed with coeliac disease also suffer from autoimmune thyroid disease. It is therefore recommended that if you are diagnosed with either of these conditions, you should be tested for the other.


The Australian Thyroid Foundation
For more information
contact The Australian Thyroid Foundation
Type 1 diabetes
Diabetes is a condition where the body is unable to regulate the amount of glucose in the blood. Insulin, produced in the pancreas, is responsible for transporting glucose from the blood to the body’s cells to be used as energy. In those with diabetes, either insufficient insulin is produced by the pancreas (type 1 and LADA (Latent Autoimmune Diabetes in the Adult)), or the insulin produced does not work properly (type 2).
Type 1 diabetes and LADA are autoimmune diseases associated with coeliac disease. Type 1 diabetes is usually diagnosed in children and young adults, while LADA usually appears in adult life. Up to 10% of children and adolescents with type 1 diabetes also have coeliac disease, most often diagnosed during routine screening.
There is no ‘official’ link between coeliac disease and type 2 diabetes, however the chronic systemic inflammation associated with undiagnosed coeliac disease may put some people at higher risk of developing metabolic diseases including type II diabetes.
Coeliac Australia and Diabetes NSW/ACT have developed these resources for people with both coeliac disease and diabetes:
Download the guide
healthy living with coeliac disease and diabetes including tips and suggestions and the gluten free carbohydrate list.


Dermatitis herpetiformis
What is dermatitis herpetiformis?
Dermatitis herpetiformis (DH) is a chronic skin condition associated with coeliac disease. It is intensely itchy, even when only appearing as a mild rash. The name, dermatitis herpetiformis, is a descriptive name. The rash is not related to either dermatitis or herpes, but is a specific chronic skin condition.
DH has a genetic basis and is not contagious. The rash may be small lumps, like insect bites, some with tiny fluid filled blisters on top, called vesicles. However, it can also appear hive-like, persisting in one area, or pink and scaly like dermatitis.
DH can flare and subside without treatment. The rash has a characteristic distribution, over the knee caps, on the outer surface of the elbows, on the buttock area, around the ears, the shoulder blades and in the hairline and eyebrows. It tends to appear symmetrically on both the left and right sides of the body. When the rash subsides, which often occurs spontaneously, it may leave brown pigmentation or pale areas where pigmentation is lost.
Who gets dermatitis herpetiformis?
People are born with a genetic predisposition to develop coeliac disease and/or DH. DH is slightly more common in males than females and generally presents in adult life (15-55 years). It is uncommon to see DH in children, but it can occur.
Less than 10% of patients with DH will also have the gastrointestinal symptoms associated with coeliac disease. However, biopsies show that people with DH will have some degree of villous atrophy (small bowel damage) on consumption of a high gluten load. There is a small group of patients with coeliac disease who later develop DH even though they have been on a strict gluten free diet for years.
Like coeliac disease, it is unclear why the condition develops at a particular time. Both genetic and environmental factors play important roles in DH.
Does dermatitis herpetiformis occur in families?
About 10% of patients with DH have first degree relatives with either DH or coeliac disease. There is the possibility that atypical or silent coeliac disease could be undiagnosed in the families of patients with DH.
How is the condition diagnosed?
The variable presentation of the rash can make diagnosis very difficult, and a referral to a dermatologist is required. When your doctor suspects DH, a skin biopsy for histopathology and immunofluorescence is performed. This involves taking a small piece of skin, which is sent to a pathologist for testing.
The sample of skin will often include a small papule and blister and some normal surrounding skin. With DH the immunofluorescence test will show deposits of IgA in the skin. Whilst IgA can be found in the skin in other skin diseases, a particular pattern in the IgA immunofluorescence is seen in DH. A positive immunofluorescence test can be obtained in many patients with DH even when the skin disease is in remission and the rash is not visible. There are also a number of abnormal serum (blood) antibodies that occur in DH, just as they do in coeliac disease.
How is the condition treated?
is treated in the same way as coeliac disease, by maintaining a strict gluten free diet for life. It may take six months to achieve moderate improvement in the skin condition and up to two years or more to achieve total control by diet alone.
An oral medication called Dapsone is available to relieve the rash of DH. Within twenty-four hours of taking this medication, the itch is often better and the rash may disappear within a few days. Dapsone, however, does not improve the small bowel damage.
Dapsone is generally well tolerated but requires careful medical supervision. It has a number of side effects, especially if taken in large amounts for long periods of time, e.g. haemolysis resulting in anaemia and chronic tiredness. Sulphapyridine and other sulphonamides are also used. Maintaining a strict gluten free diet is essential to reducing and eliminating the use of medication. Even occasional unintentional gluten intake reduces successful elimination of Dapsone for many patients. Where compliance with the gluten free diet is strict, the average time for reduction in the use of Dapsone has been shown in one study to be less than a year and can generally be stopped within about two years.
What are the implications of dermatitis herpetiformis?
The implications of DH are the same as for coeliac disease.
-
Before diagnosis, both DH and coeliac patients may suffer from nutritional deficiencies caused by malabsorption (link to previous page). .
-
There is a small, but statistically higher risk of developing lymphoma, particularly when the condition has been untreated for many years. .
-
Patients with DH, particularly females, have an increased risk of autoimmune thyroid disease. Twenty per cent of patients with DH have clinical hypothyroidism and about 10% have asymptomatic goitres. .
Osteoporosis
What is osteoporosis?
Osteoporosis is a condition in which the bones become fragile and brittle, leading to a higher risk of fracture than in normal bone. There are no obvious symptoms of osteoporosis until a fracture occurs. Consequently, a person will not know that they have osteoporosis unless it is diagnosed by clinical tests or if they have an osteoporotic fracture.
How is osteoporosis related to coeliac disease?
Osteoporosis can be caused by the chronic inflammatory process in untreated coeliac disease which impairs how well the body can lay down new bone. Moreover, when the small bowel is damaged by coeliac disease, insufficient calcium and vitamin D can be absorbed.
Calcium is the key mineral that contributes to bone strength and plays a vital role at a cellular level within the body’s tissues and fluids. This requires a stable blood level of calcium.
Additionally, Vitamin D is a critical hormone that improves calcium absorption and is important for bone health. If insufficient dietary calcium and vitamin D are absorbed to maintain the required level of calcium in the blood, more is taken from the bones than can be replaced, leading to a loss of bone density.
Untreated coeliac disease will impact on a growing child and mean their bones may not reach optimal bone mass. Early diagnosis and treatment of coeliac disease is important to avoid this complication.
Over 1 million Australians have osteoporosis – resulting in over 183,000 broken bones each year. Early diagnosis and treatment can reduce the impact of osteoporosis.
How can I be tested for osteoporosis?
Osteoporosis is diagnosed with a bone density scan (or DEXA scan). It is a simple scan that measures the density of your bones at the hip and spine. You simply lie on a flat padded table, and the arm of the machine passes over your body. The scan takes approximately 10-15 minutes. You remain clothed during the scan. Results from the test will be sent to your doctor.
Medicare rebate
A person medically diagnosed with coeliac disease is entitled to a Medicare rebate, every two years, for a bone density measurement under item number 12315, ‘a proven malabsorptive disorder’. Ask the provider what their charges are at the time of booking your appointment, and whether this is the scheduled fee covered by the rebate, as there can be an out-of-pocket expense with some providers.
How often do I need to have a bone density test?
All adults diagnosed with coeliac disease should have their bone density checked as soon as possible after diagnosis. It is recommended this be repeated every 5 years, or more regularly is required. Where possible, it is important to have your bone density test repeated on the same bone densitometer at the clinic or hospital you attended for your initial visit, as there can be slight differences in results obtained on different machines.
What is the treatment for osteoporosis?
Adequate dietary calcium and weight bearing exercises are essential to prevent further bone loss. Smoking and a high intake of alcohol should be avoided. Additional treatments are often recommended, including specific, effective, medications. Speak to your doctor about the different treatments for osteoporosis.


Lactose Intolerance
Lactose is the carbohydrate (or sugar) found naturally in milk. People with lactose intolerance don’t produce enough lactase (the enzyme that digests lactose), resulting in lactose maldigestion. Symptoms of lactose maldigestion may include abdominal pain, bloating, wind and/or diarrhoea.
Untreated coeliac disease can affect lactase production and result in a temporary lactose intolerance.
The gluten free diet allows inflammation in the gut to settle, and lactase production often returns to normal. If you were intolerant to lactose prior to being diagnosed with coeliac disease, you may like to experiment with small amounts after being on the gluten free diet for a while, to see if your intolerance has resolved.
Note: It is possible for lactose intolerance to occur independently of coeliac disease e.g. due to age, ethnicity, etc. In these cases, the lactose intolerance will probably persist despite the gluten free diet.
Managing lactose intolerance
Untreated coeliac disease can affect lactase production and result in temporary lactose intolerance. The gluten free diet allows lactase production to return to normal and the lactose intolerance to resolve.
Remember: It is possible for lactose intolerance to occur independently of coeliac disease, e.g. due to age, ethnicity, etc. In these cases, the lactose intolerance will persist despite the gluten free diet.
Lactose intolerance does not cause gut damage in the same way as coeliac disease. Managing the condition involves reducing lactose containing foods to control symptoms.
If you have lactose intolerance, you DO NOT need to avoid all dairy foods. Some dairy foods are high in lactose (e.g. cow’s milk, ice cream and cream), and others contain virtually none (e.g. lactose-free milks, hard cheeses, butter, kefir and whey protein isolate).
You can effectively include all dairy foods in your diet in varying amounts, according to your individual level of tolerance.
You can also experiment with products such as ‘lacteeze’ which you can add to higher-lactose dairy products to degrade the lactose before digestion.
Here are some other tips to get your three serves of dairy each day while reducing your lactose intake:
- Consume lactose containing food/drinks in combination with other foods (not on an empty stomach)
- Start with small amounts and gradually increase your consumption to build tolerance
- Spread your lactose containing food/drinks out over the day
- Regular (full cream) milk contains less lactose than low fat or skim milk
- Yoghurt (especially probiotic yoghurts) may be well tolerated (the bacteria in yoghurt break down the lactose over time)
The lactose content of some dairy products
-
Dairy Food
Lactose Content (g)
-
Regular Milk (250mL)
11.8
-
Cheddar Cheese (40g)
0.0
-
Swiss Cheese (40g)
0.1
-
Parmesan Cheese (40g)
0.0
-
Brie Cheese (40g)
0.1
-
Ricotta Cheese (20g)0.24
0.24
-
Cream Cheese (22g)
0.6
-
Natural Yoghurt (200g)
9.4
-
Ice Cream (50g)
2.8
-
Butter (1 Tablespoon)
0.1
-
Cream (1 Tablespoon)
0.6
Dairy Australia & The Gut Foundation 2005
Consult an Accredited Practising Dietitian to help you manage your diet.